Imagine being able to know if you have Parkinson’s disease, multiple sclerosis, liver failure, Crohn’s diseases, pulmonary hypertension, chronic kidney disease, or any number of cancers based on a simple, non-invasive test of your breath? Breath analyzers to detect alcoholhave been around for well over half a century—why not apply the same concept to detect diseases? A global team of scientists from universities in Israel, France, Latvia, China and the United States have developed an artificial intelligence (AI) system to detect 17 diseases from exhaled breath with 86 percent accuracy.
The research team led by Professor Hassam Haick of the Technion-Israel Institute of Technology collected breath samples from 1404 subjects with either no disease (healthy control) or one of 17 different diseases. The disease conditions include lung cancer, colorectal cancer, head and neck cancer, ovarian cancer, bladder cancer, prostate cancer, kidney cancer, gastric cancer, Crohn’s disease, ulcerative colitis, irritable bowel syndrome, idiopathic Parkinson’s, atypical Parkinson ISM, multiple sclerosis, pulmonary hypertension, pre-eclampsia toxemia, and chronic kidney disease.
The concept is relatively simple—identify breathprints of diseases, and compare it to human exhalation. What makes it complicated is the execution of the concept. For example, how to identify the breathprint of a disease? Is it unique like a fingerprint? To answer this question requires a deeper look at the molecular composition of breath.
When we exhale, nitrogen, oxygen, carbon dioxide, argon, and water vapor are released. Human breath also contains volatile organic compounds (VOCs)–organic chemicals that are emitted as gases, and have a high vapor pressure at normal temperature. American biochemist Linus Pauling, one of the founders of modern quantum chemistry and molecular biology, and recipient of the 1954 Nobel Prize in Chemistry, and the 1962 Nobel Peace Prize, studied 250 human breath volatiles using a gas-liquid chromatogram in 1971. Pauling is widely regarded as a pioneer in modern breath analysis. Exhaled breath contains approximately over 3,500 components mostly comprised of VOCs in small quantities according to a 2011 study published in “Annals of Allergy, Asthma & Immunology.”
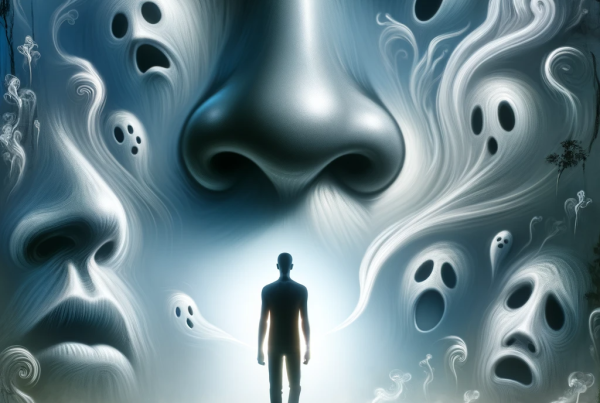
VOCs are the common factor in the smelling process for both breath analyzers and humans. When we inhale, the nose draws in odor molecules that typically contain volatile (easy to evaporate) chemicals. Once the odor molecules contact the olfactory epithelium tissue that lines the nasal cavity, it binds with the olfactory receptors and sends an electrical impulse to a spherical structure called the glomerulus in the olfactory bulb of the brain. There are approximately 2,000 glomeruli near the surface of the olfactory bulb. Smell is the brain’s interpretation of the odorant patterns released from the glomerulus. The human nose can detect a trillion smells. In Haick’s researcher team, nanotechnology and machine learning replaces the biological brain in the smelling process.
Haick’s team of scientists developed a system, aptly called “NaNose,” that uses nanotechnology-based sensors trained to detect volatile organic compounds associated with select diseases in the study. NaNose has two layers. One is an inorganic nanolayer with nanotubes and gold nanoparticles for electrical conductivity. The other is an organic sensing layer with carbon that controls the electrical resistance of the inorganic layer based on the incoming VOCs. The electrical resistance changes depending on the VOCs.
Efforts are underway to miniaturize and commercialize the innovative technology developed by Haick’s team in a project called “SniffPhone.” In November 2018, the European Commission’s Horizon 2020 awarded the SniffPhone the “2018 Innovation Award” for the “Most Innovative Project.”
The market opportunity for medical breath analyzers is expected to grow. By 2024, the breath analyzer market is projected to increase to USD 11.3 billion globally according to figures published in Jun 2018 by Grand View Research—alcohol detection has a majority of the revenue share. Currently breath analyzers are used to detect alcohol, drugs, and to diagnose asthma and gastroenteric conditions. Clinical applications are projected to increase due to the introduction of “introduction of advanced technologies to detect nitric oxide and carbon monoxide in breath,” Grand View Research states. According to the study, the medical application segment is expected to grow due to ability of breath analyzers to detect volatile organic compounds (VOCs) that may help in “early diagnosis of conditions including cardiopulmonary diseases and lung and breast cancer,” and act as “biomarkers to assess disease progressions.”
By applying cross-disciplinary innovative technologies from the fields of artificial intelligence, nanotechnology, and molecular chemistry, diagnosing a wide variety of diseases may be as simple and non-invasive as a breath analysis using a handheld device in the not-so-distant future.
Copyright © 2019 Cami Rosso All rights reserved.
References
Nakhleh, Morad K. , Amal, Haitham , Jeries, Raneen , Broza, Yoav Y. , Aboud, Manal , Gharra, Alaa , Ivgi, Hodaya, Khatib, Salam, Badarneh, Shifaa, Har-Shai, Lior, Glass-Marmor, Lea, Lejbkowicz, Izabella, Miller, Ariel, Badarny, Samih, Winer, Raz, Finberg, John, Cohen-Kaminsky, Sylvia, Perros, Frédéric, Montani, David, Girerd, Barbara, Garcia, Gilles, Simonneau, Gérald, Nakhoul, Farid, Baram, Shira, Salim, Raed, Hakim, Marwan, Gruber, Maayan, Ronen, Ohad, Marshak, Tal, Doweck, Ilana, Nativ, Ofer, Bahouth, Zaher, Shi, Da-you, Zhang, Wei, Hua, Qing-ling, Pan, Yue-yin, Tao, Li, Liu, Hu, Karban, Amir, Koifman, Eduard, Rainis, Tova, Skapars, Roberts, Sivins, Armands, Ancans, Guntis, Liepniece-Karele, Inta, Kikuste, Ilze, Lasina, Iev, Tolmanis, Ivars, Johnson, Douglas, Millstone, Stuart Z., Fulton, Jennifer, Wells, John W. , Wilf, Larry H., Humbert, Mar, Leja, Marcis, Peled, Nir, Haick, Hossam. “Diagnosis and Classification of 17 Diseases from 1404 Subjects via Pattern Analysis of Exhaled Molecules.” ACS Nano. DOI: 10.1021/acsnano.6b04930. November 2017.
Scudellari, Megan.”Breathalyzer Distinguishes Among 17 Diseases at Once.” IEEE Spectrum. January 5, 2017.
Lawal, Oluwasola, Ahmed, Wagar M., Nijsen, Tamara M.E., Goodacre, Royston, Fowler, Stephen J. “Exhaled Breath analysis: a review of ‘breath-taking’ methods for off-line analysis.” Metabolomics. August 19, 2017.
Shirasu, Mika, Touhra, Kazushige. “The scent of disease: volatile organic compounds of the human body related to disease and disorder.” The Journal of Biochemistry. September 1, 2011.
The Nobel Prize. “Linus Pauling.” Retrieved 1-29-2019 from https://www.nobelprize.org/prizes/peace/1962/pauling/facts/
Pauling, Linus, Robinson, Arthur B., Teranishi, Roy, Cary Paul. “Quantitative Analysis of Urine Vapor and Breath by Gas-Liquid Partition Chromatography.” PNAS. October 1971.
Phillips, Michael. “Breath Tests in Medicine.” Scientific American. July 1992.
Popov, Todor A. “Human exhaled breath analysis.” Annals of Allergy, Asthma & Immunology. January 22, 2011.
Bushak, Lecia. “How Does The Nose Smell? The Inner Workings of Our Sense Of Smell.” Medical Daily. March 5, 2015.
Williams, Sarah C.P. “Human Nose Can Detect A Trillion Smells.” Science. March 20, 2014.
SniffPhone.”SniffPhone wins 2018 Innovation Award.” Retrieved from https://www.sniffphone.eu/
Grand View Research. “Breath Analyzers Market Size, Share & Trends Analysis Report By Technology (Fuel Cell, Semiconductor Sensor, Infrared Spectroscopy), By Application (Alcohol Detection, Medical), And Segment Forecasts, 2018 – 2024.” June 2018. Retrieved from https://www.grandviewresearch.com/industry-analysis/breath-analyzer-market
Source: Innovative AI Breath Analyzer Diagnoses Diseases by “Smell”