A trainee presenting a case told me the patient’s urine smelled like cancer. Back up here! What do you mean, I asked him? But no matter how hard he tried, he couldn’t put it into words. It just does, he said.
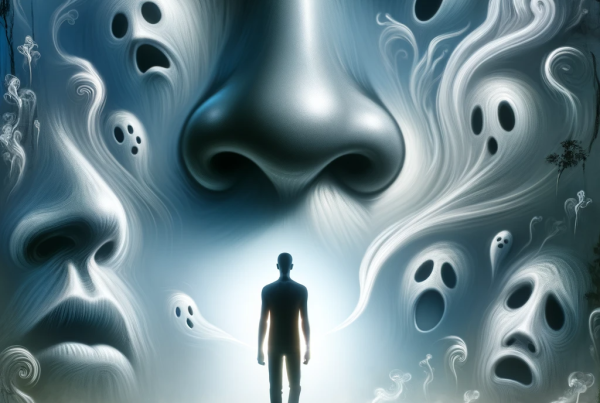
Smell is certainly one of our odder senses. It’s the most ancient, visceral, and probably evolutionarily important senses. Unlike the other senses, once the olfactory receptors are triggered by whatever odor molecules we have the good or bad fortune to sniff, the neuronal journey is rapid and takes little detour. It sparks directly down a path to the buried, atavistic, and darker recesses of our brain, primarily the limbic system, the real estate responsible for behavior, emotion, and memory.
Most of this happens without input from that showy newcomer, the cortex. This means that our perception of smell is often immediate, emotive, and automatic. And it has left us with an interesting paucity of language when it comes to describing smells. We can describe what we see in infinitely elaborate language, rich in metaphor and descriptors, but smells are usually only described in terms of, well, other smells (unless you are Ray Bradbury: “She smelled the way the Taj Mahal looks by moonlight”). Smells trigger memory, as you all have experienced. As Diane Ackerman wrote, “Smells detonate softly in our memory like poignant land mines.”
It is likely that an acute sense of smell was vital in mammalian evolution. After all, our only job as organisms is to survive and procreate, so smell alerted us to danger—distinguishing kin from predator, allowing us to detect food gone bad, and letting waft in the pheromones with their promise of Neanderthal romance, potential mates having a rather seductive odor fingerprint. Animals down the evolutionary food chain have far better senses of smell than we gawky humans. Dogs, in particular, which we will come to in a minute.
Sniffing Out Disease
We emergency clinicians and our long-suffering olfactory bulbs are no stranger to the power of smell. Who among us has not been able to diagnose diabetic ketoacidosis, uremia, and pseudomonal infection from the end of a cubicle? A vast number of diseases are recognizable from their volatile signature, even if we and our underdeveloped sniffs cannot put a finger on it. Like the uncanny valley of fragrance, when something appears just a little off, we presume it is sick and are repulsed by it, lest we associate, or even worse, mate with it.
The physiological details of how we smell are vast and, sadly, beyond the scope of this column. A few snippets worth mentioning are the fact that odor molecules must be volatile, aerosolized, and in need of gravity even to start the process (it’s harder to smell in space!). Once in contact with the intricate bulbs, huge swaths of messaging and signaling and transport functions set off like starbursts. We have spatial arrangement of smells (although, again, not as good as dogs, who only need five footsteps to establish a smell trail).
Anosmia, of course, is a hot topic right now. The loss of the sense of smell rocketed out of the expanse of information we were receiving concerning the pathological sequelae of coronavirus infection. We’ve always known that certain disease states can induce anosmia: infectious pathogens causing sino-nasal disease, trauma, neurodegenerative conditions, but never has this symptom been such a neon signpost. Exact numbers of how frequently anosmia occurs in COVID-19 are still unclear. Our data remain rough and emerging, but it will be well over 50 percent in more minor presentations and much higher in the sicker cohorts.
From a pathophysiological viewpoint, the nasal epithelial cells have a high expression of angiotensin-converting enzyme 2 receptor, the nasal welcome mat for the coronavirus. The anosmia may be long-term and debilitating (more so for its role in hypogeusia, the impoverishing reduction in taste and enjoyment of food), but there are, surprisingly, treatments. Olfactory training is recommended. This consists of deliberately sniffing four essential oils (rose, lemon, clove, and eucalyptus) for 20 seconds each twice a day. It is recommended that the oils are changed for others each month. The understanding is that this is perhaps retraining other neurons to carry the heavy burden of smells back into the labyrinth of the brain.
The Irony of It
But let us return to the noblest of creatures, dogs. I recently read an article discussing a Finnish airport’s pilot program of using dogs to sniff out the coronavirus. At this stage, their accuracy is impressive, and any identified positives are then referred for conventional testing. The dogs are trained by the fabulously named Nose Wise, a smell detection agency. The UK is undergoing similar research under the charity Medical Detection Dogs. Canines have already shown excellent ability to sniff out certain cancers, Parkinson’s disease, and malaria. There is a certain irony in using smell to root out a disease that destroys smell.
I wanted to end this column having made the argument that we really need dogs in every emergency department, but I shall instead leave you with some odor-related literature. Helen Keller was considered a prodigy of smell. “The sense of smell has told me of a coming storm hours before there was any sign of it visible. I notice first a throb of expectancy, a slight quiver, a concentration in my nostrils.”
Dr. Johnstonis a board-certified emergency physician, thus the same as you but with a weird accent. She works in a trauma center situated down the unfashionable end of Perth, Western Australia. She is the author of the novel Dustfall, available on her website, http://michellejohnston.com.au/. She also contributes regularly to the blog, Life in the Fast Lane, https://lifeinthefastlane.com. Follow her on Twitter@Eleytherius, and read her past columns at http://bit.ly/EMN-WhatLiesBeneath.
Source: What Lies Beneath: Olfaction in the Time of COVID-19 : Emergency Medicine News