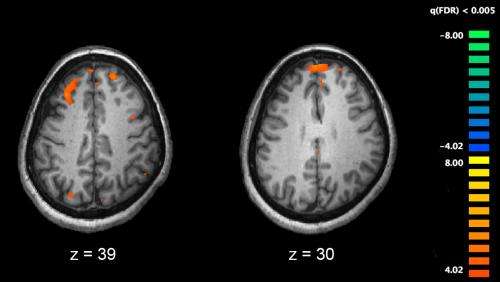
Functional magnetic resonance imaging (fMRI) and other brain imaging technologies allow for the study of differences in brain activity in people diagnosed with schizophrenia. The image shows two levels of the brain, with areas that were more active in healthy controls than in schizophrenia patients shown in orange, during an fMRI study of working memory. Credit: Kim J, Matthews NL, Park S./PLoS One.
Schizophrenia is associated with a wide range of cognitive impairments including sensory information processing. Findings showed that impaired sensory processing, either hypo- or hyper-reactivity to sensory stimuli, is an important marker contributing to the development of psychotic symptoms and cognitive impairments of schizophrenia. Most of the previous studies have primarily focused on the investigation of cognitive processing and neural mechanism of sensory information processing in schizophrenia.
However, it is equally important to understand how specific sensory responsiveness patterns are with the symptomatology of schizophrenia. Moreover, given that schizophrenia and autism are neurodevelopmental disorders having shared cognitive and social dysfunctions, and showing high co-occurrence rates, it is important for us to examine the uniqueness and similarities in sensory responsiveness between patients with schizophrenia and autism. Such an altered sensory responsiveness is much neglected in the extant literature.
Dr. Raymond Chan’s team from the Institute of Psychology has conducted a study to examine sensory responsiveness in 98 typically developing adolescents and 29 adolescents with early onset schizophrenia. They also examined the relationship between schizotypal traits and sensory responsiveness patterns between these two groups.
They administered the Adult/Adolescent Sensory Profile, the Schizotypal Personality Questionnaire and the Autism Spectrum Quotient to all participants.
Their findings showed that higher levels of hypersensitivity and hyposensitivity coexisted in adolescent with early onset schizophrenia and were correlated with positive and negative symptoms of schizophrenia. Positive correlation was found between atypical sensory experiences and higher levels of schizotypal traits.
Interestingly, the strength and pattern of such correlations were found to be comparable in both adolescents with early onset schizophrenia and typically developing adolescents.
Moreover, higher levels of autistic traits would intensify the positive correlation between schizotypal traits and sensory responsiveness abnormalities, suggesting an additive effect of co-occurring schizotypal and autistic traits on atypical sensory experiences.
“These findings contribute to our understanding of the altered sensory responsiveness patterns in early onset schizophrenia. Importantly, these findings may also help us to develop appropriate sensory-related interventions in patients with neurodevelopmental disorders,” said Dr. Chan.
This study has been published in a paper in the Journal of Psychiatric Research entitled “Self-reported sensory responsiveness patterns in typically developing and early onset schizophrenia adolescents: its relationship with schizotypal and autistic traits.”
Explore further
More information: Han-yu Zhou et al. Self-reported sensory responsiveness patterns in typically-developing and early-onset schizophrenia adolescents: Its relationship with schizotypal and autistic traits, Journal of Psychiatric Research (2020). DOI: 10.1016/j.jpsychires.2020.10.002
Source: Research illustrates atypical sensory experiences in early-onset schizophrenia adolescents