Aromatherapy is a relatively safe, all-natural use of essential oils to support one’s health.
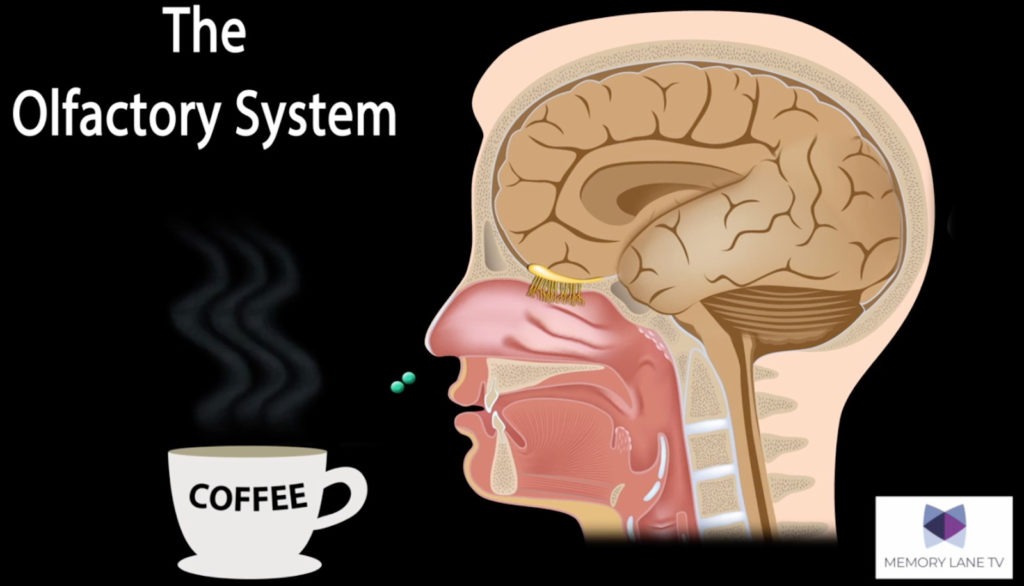
Although research has shown that a person’s sense of smell may decrease as Alzheimer’s disease progresses, the nose is still an entryway for the sensory stimuli of essential oils because the nasal cavity and nerve cells in the nasal lining are the closest entry to the limbic system. This connection between the sense of smell and the limbic system accounts for the influence of essential oils on mood and memory.
Using essential oils can aid in efforts to restore the body back to its natural balance. For example, if you’re feeling sad, they may help you feel content; if you are feeling anxious, they may help you relax. Essential oils can be diffused in the air, placed on stoned jewelry, or applied to pulse points around the neck and wrist areas, like perfume or cologne. Within 20 seconds of inhaling, an essential oil will start to work. And by 30 minutes they have traveled throughout the whole body.
Many clinical trials support the effectiveness of essential oils, including lavender and cedar for reducing anxiety and peppermint for mental stimulation. Essential oils may also be used to stimulate the appetite, help with sleep, increase energy, improve attention and concentration, and much more.
The newest empirically-validated framework that includes the use of aromatherapy is the Dementia Connection Model©.
The Dementia Connection Model is a cognitive-behavioral framework that takes into account how the person living with dementia is progressing through their disease, focusing on what we know works well with advancing dementia — sensory stimulation.
When a person with dementia is stimulated using their senses, that information is processed either directly or indirectly in the limbic system of their brain that houses the amygdala (feelings) and hippocampus (memories). Therefore, positive stimuli should be used to promote positive feelings and memories, encouraging positive behavioral expressions. And when the caregiver is the one providing these positive experiences, the person with dementia will either connect or re-connect with them because they like how they feel with that person.
Within the Dementia Connection Model comes an approach to care called The Perfect Day™. Each part of the day (i.e., morning, mid-day, afternoon/evening), specific sensory stimuli should be used to encourage positive behavioral expressions and minimize sundowning behaviors. These various sensory stimuli include auditory stimulation with music, olfactory stimulation with aromatherapy, tactile stimulation with exercise, pets, dolls, and more, and so on.
A published review from 2019 provides an excellent summary of studies supporting the therapeutic use of essential oils in people with Alzheimer’s disease specifically. In The Perfect Day method, the recommendation to help curb unproductive and negative behavioral expressions and sundowning includes using peppermint and a citrus scent in the morning. This helps increase mental clarity, and is great for a morning time regimen; citrus additionally increases appetite and improves mood.
At meal times, citrus scents should be used to encourage eating and keep the “mood of the room” elevated. Then, about 30 minutes prior to sundowning and through the afternoon and evening, lavender should be used to promote a sense of calm and encourage sleep. If the person can still smell and they don’t care for the scents being used, then simply try another essential oil that has the same benefits. Now, when this is used daily, there is an immediate effect on promoting positive feelings, memories and behaviors, however, after about four weeks, the person may associate these smells with understanding what time of day it is and what they should be doing, decreasing confusion, loneliness and fear.
It’s important to keep in mind that any substance with a fragrance, including essential oils, may cause an allergic reaction in individuals with sensitivities. Use caution and test a small amount of the oil when introducing it. You will want to consult with your loved one’s healthcare practitioner and be sure to mention any essential oils and other supplements that you may be using or want to use.
This aromatherapy approach fits nicely with pleasing auditory and visual sounds, like with Memory Lane TV. Based on scientific evidence, Memory Lane TV is another recent, multi-sensory standard used in the industry to manage behavioral symptoms using media stimulation and artificial intelligence.
Building on pre-existing research focused on the impact of sensory stimulation, Memory Lane TV has produced over 500 hours of scientifically designed film montage with elements of music, soundscapes, video sequences and still images to induce a variety of responses in the viewer, such as anxiety stress-reduction, re-grounding to combat sundowning, increased appetite, improved engagement, memory activation and other positive benefits.
Geriatric physicians, occupational therapists, long-term care providers and memory care research centers were involved in the design of the intervention. Media stimulation has wonderful potential as an additional tool for dementia care. At the Benson-Henry Institute for Mind Body Medicine at Massachusetts General Hospital, Herbert Benson, MD, the noted inventor of the relaxation response, described the effect of Memory Lane TV as a way to demonstrate the effectiveness of the relaxation response on a specific pathology that impact the brain, i.e., dementia.
After eight years of gathering data about the efficacy of the intervention, we have identified three main benefits of sensory stimulation in long-term care or at home:
- It increases respite opportunity
- It decreases stress and anxiety
- It improves interaction with a person with whom care partners are caring for
Memory Lane TV integrates audio, visual and olfactory stimulation by design. The content is scientifically and therapeutically designed to target specific behavioral and psychological outcomes from inception. It’s not merely plot-free, and is entertaining yet should not be considered as only entertainment — it is a tool to manage effectively behavioral symptoms associated to memory loss and improve the quality of life through guided imagery and reminiscence. The service is designed to be equally effective, accessible, and affordable both in home and professional settings.
And recent research is showing that multi-sensory stimulation can also have an impact on reducing psychotropics and improving engagement. All that increases productivity and staff quality of care, but also offers a hedge to institutions that use that type of evidence-based, non-pharmacological intervention.
All-in-all, olfactory stimulation should be included as part of any holistic plan of care or simply just daily use for those living with dementia.
Jennifer Stelter, Psy.D., CDP, CADDCT, is the co-owner of NeuroEssence, LLC at the Dementia Connection Institute and the author of “The Busy Caregiver’s Guide to Advanced Alzheimer Disease” published by Johns Hopkins Press.
Jennifer Ryan, BS, CDP, is the co-owner of NeuroEssence, LLC and an educator and master trainer for the Dementia Connection Specialist Certified Trainer (DCSCT) Certification Program.
Alban Maino is the CEO of Memory Lane TV.
The opinions expressed in McKnight’s Long-Term Care News guest submissions are the author’s and are not necessarily those of McKnight’s Long-Term Care News or its editors.
Source: Something smells…and I like it – Marketplace Experts – McKnight’s Long-Term Care News