Sensory neurons pick up information from our senses and relay it to the rest of the nervous system. But this is not their only mission. In a new study published in the journal Current Biology, Claire Wyart at the Paris Brain Institute, and Christina Vandenbroucke-Grauls at the Amsterdam University Medical Centers, have shown that sensory neurons in the central nervous system play a leading role in pneumococcal meningitis, a severe infection with a high mortality rate and strong epidemic potential. They help fight infection and promote host survival.
“Studies at Harvard University have shown that sensory cells in the skin can help fight infection when bacteria invade subcutaneous tissue,” says Claire Wyart, head of the Spinal Sensory Signaling team at the Paris Brain Institute. “The same phenomenon occurs in the event of a respiratory infection: ciliated cells detect the trace of pathogenic bacteria and trigger an inflammatory reaction. We wanted to find out if there was a similar protective system in the central nervous system.”
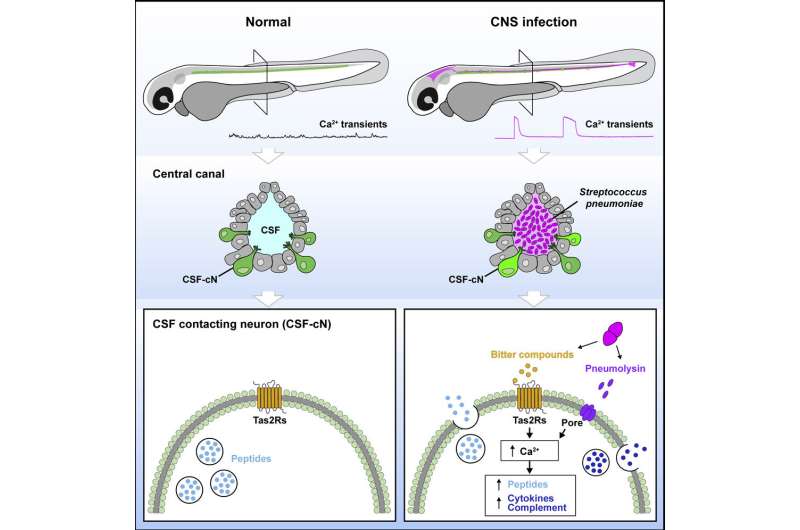
To this end, the researchers looked at the role of sensory cells located along the walls of the central canal in the spinal cord. Known as cerebrospinal fluid-contacting neurons, or CSF neurons in short, they are numerous across vertebrate species. These neurons can detect spinal curvature in real time and use this information to adapt the body’s posture to accomplish challenging motor tasks. Over the past 10 years, Claire Wyart’s team has shown that this detection system optimizes posture and locomotion during physical activity. But it also adjusts the spine’s shape throughout life, growth, and aging.
“We suspected that these neurons were involved in meningitis, a disease characterized by inflammation of the meninges—the membranes that envelop the brain and spinal cord,” she explains. “In pneumococcal meningitis, in particular, the pathogenic bacterium Streptococcus pneumoniae invades the cerebrospinal fluid that circulates from the ventricles of the brain to the central canal of the spinal cord… precisely where cerebrospinal fluid-contacting neurons are located. Infected patients also show significant neck stiffness; if left untreated, this leads to a characteristic posture change called opisthotonos, in which the back is exaggeratedly arched. With all these clues in hand, we had to investigate.”
Modulating inflammation and immune response
To understand the role of these cells in pneumococcal meningitis, the researchers used an animal model of the disease. After injecting Streptococcus pneumoniae into the hindbrain of zebrafish larvae, they observed that the symptoms of meningitis in animals were reminiscent of the disease’s clinical manifestation at an advanced stage. In particular, the fish had abnormal dorsal curvature and epileptic-like seizures.
“We found that CSF neurons became extraordinarily activated once the pathogenic bacteria had entered the cerebrospinal fluid and invaded the spinal cord’s central canal,” says Wyart. The indicator of this activation? Massive calcium transients. The researchers also observed these transients in vitro as soon as sensory neurons were exposed to secretions of Streptococcus pneumoniae—which are recognized as bitter substances.
“CSF neurons express taste receptors; They literally taste bitterness! We knew that bitterness receptors played an important role in oral immunity because they detect contaminated food before ingestion. But not that they were involved in brain infections,” says the researcher.
“These sensory neurons are surprising: during an infection, they taste the content of the cerebrospinal fluid, spot intruding bacteria through bitterness receptors, then increase the expression of cytokines and other proteins involved in innate immunity—the first line of defense against pathogens.”
To verify that contact neurons contribute to the immune response in pneumococcal infection, the researchers removed them in zebrafish larvae—reducing their lifespan and increasing the level of bacteria in their bodies.
Meningitis, a dreaded disease
Streptococcus pneumoniae is the most common cause of community-transmitted meningitis. The disease affects about 500,000 people a year and is associated with high mortality, particularly in sub-Saharan Africa, according to WHO. It has an annual incidence is 1–3 cases per 100,000 people in industrialized countries where vaccines are available. In addition, it causes brain damage due to infection and the host’s inflammatory response.
“This is not the only form of meningitis in which contact neurons are involved,” says Wyart. “Our results show that the bitterness receptors expressed by these cells also recognize Listeria monocytogenes, another primary source of infection, and a neurotropic virus called Sindbis. We think they can detect many other pathogens. Ultimately, a better understanding of these sensory neurons may allow us to open therapeutic avenues for other nervous system infections, for which we do not yet have any vaccines.”
More information: Andrew E. Prendergast et al, CSF-contacting neurons respond to Streptococcus pneumoniae and promote host survival during central nervous system infection, Current Biology (2023). DOI: 10.1016/j.cub.2023.01.039
Other references:
Jenna R. Freund et al, Activation of airway epithelial bitter taste receptors by Pseudomonas aeruginosa quinolones modulates calcium, cyclic-AMP, and nitric oxide signaling, Journal of Biological Chemistry (2018). DOI: 10.1074/jbc.RA117.001005.
Deepak A Deshpande et al, Bitter taste receptors on airway smooth muscle bronchodilate by localized calcium signaling and reverse obstruction, Nature Medicine (2010). DOI: 10.1038/nm.2237
Robert J. Lee et al, Taste receptors in innate immunity, Cellular and Molecular Life Sciences (2014). DOI: 10.1007/s00018-014-1736-7
Source: Sensory cells taste cerebrospinal fluid to fight brain infections